Post updated January 2021.
Why are we still telling people that they must be at least 75-100 pounds overweight before they can have bariatric surgery—the most effective way to lose weight?
Other methods for losing weight—diet and exercise—are largely not effective long term. Diet and exercise programs fail for 95-98% of people within 3 years.1,2 In fact, up to 66% of those dieters end up even heavier than they were before.1
Why is this the case? It’s because of an inconvenient biological fact: the body weight set point.
To understand this set point, think of the thermostat in your home. Let’s say it’s set at 68°. When the temperature in your home drops, the heat kicks on, because the thermostat’s job is to keep your home at that 68° at which it’s set.
Your body acts much the same way as your thermostat. When you start losing weight through diet and exercise, your body kicks into gear to defend itself against this (perceived) threat to your health! It increases your appetite so you want to eat more calories, and decreases your metabolism so you don’t burn them off so fast.3
The sad fact is that while many people can lose weight in the short term with diet and exercise, they struggle to maintain that loss. It’s not willpower; it’s biology. And biology is not on our side when it comes to losing weight.
So if we know that diet and exercise programs don’t work for lasting weight loss…why are we preventing people from accessing a tool that does work?
Bariatric surgery works for weight loss, because unlike diet and exercise, it changes the body weight set point. I encourage you to read my blog post about this fascinating science: Weight Loss Surgery Changes Body Weight Set Point.
We know that mild obesity, also known as class 1 obesity, or low BMI obesity (BMI 30-35, typically 50-75 pounds over ideal weight), can still lead to serious medical problems, hinder quality of life, and shorten lifespan. Calculate my BMI here.
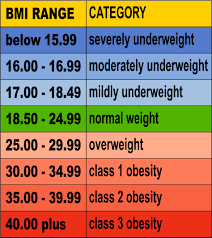
Yet often bariatric surgery is only recommended for people who have a BMI greater than 35. Yet a person is considered obese at BMI 30! Are we really asking people to gain more weight before they can use the tool that works?
The truth is that the recommendations about who can (or can’t) have bariatric surgery are outdated and need to change.
Health insurance companies still follow the NIH Guidelines for weight loss surgery
The NIH guidelines for weight loss surgery state that bariatric surgery can be considered for patients who have a BMI greater than 40, or a BMI greater than 35 with major weight-related medical problems (such as diabetes).
Those guidelines were proposed in 1991—about 30 years ago. Since that time, new bariatric procedures have been introduced. Surgeries are now performed laparoscopically. Bariatric surgery outcomes have greatly improved.
We also have a better understanding of the significant danger of obesity. And mild obesity is still obesity.
The problem is that health insurance companies still follow these outdated NIH guidelines. If you don’t meet the NIH standards, your health insurance company won’t pay for the bariatric surgery.
This is unfair and needs to change.
Low BMI obesity patients deserve effective treatment, too.
What the American Society for Metabolic and Bariatric Surgery (ASMBS) has to say
In 2012, the ASMBS published a low BMI position statement in support of bariatric surgery for suitable low BMI patients (BMI 30-35, roughly 50-75 pounds overweight).
In 2018, the ASMBS published an updated low BMI position statement (PDF) expressing even stronger support, because of additional high-quality studies that had been published further demonstrating the safety and efficacy of weight loss surgery in the BMI 30-35 population.
The summary and recommendations from the 2018 position statement are as follows (paraphrased):
- Class I obesity (BMI 30–35 kg/m2) causes or exacerbates multiple other diseases, decreases longevity, and impairs quality of life. Patients with class I obesity require durable treatment for their disease.
Comment from Dr. Oliak – this is a stronger stance than the ASMBS took in 2012. In 2012, the ASMBS said that low BMI patients should be recognized as deserving treatment. In this position statement the ASMBS says that low BMI patients require durable treatment.
- Current nonsurgical treatments for class I obesity (e.g. diet, exercise programs) are often ineffective at achieving major, long-term weight reduction and resolution of weight-related medical issues.
Comment from Dr. Oliak – diet and exercise programs fail for 95-98% of people within 3 years.1,2
- The existing BMI inclusion criterion of ≥35 kg/m2 as a requirement for bariatric and metabolic surgery— excluding individuals with class I obesity—was established arbitrarily more than a quarter century ago, in the era of open surgery when complications and mortality of surgery was significantly higher than today. There is no current evidence of clinical efficacy, cost-effectiveness, ethics, or equity that justifies this group being excluded from life-saving surgical treatment. Access to bariatric surgery should not be denied solely based on this outdated threshold.
Comment from Dr. Oliak – this is a stronger statement than the ASMBS made in the 2012 position statement. In this statement, the ASMBS added the last sentence, stating that weight loss surgery should not be denied based solely on BMI being 30-35.
- For patients with BMI 30 to 35 kg/m2 and obesity-related medical issues who do not achieve substantial, durable weight loss with reasonable nonsurgical methods, bariatric surgery should be offered as an option for suitable individuals.
Comment from Dr. Oliak – this is a new and very strong statement that wasn’t made in the 2012 position statement. The ASMBS felt comfortable making this statement based on the many additional studies published after 2012 demonstrating safety and efficacy of weight loss surgery in the low BMI population.
- Particularly given the presence of high-quality data in patients with type 2 diabetes, bariatric surgery should be strongly considered for patients with BMI 30 to 35 kg/m2 and type 2 diabetes.
Comment from Dr. Oliak – this is a new and very strong statement that wasn’t made in the 2012 position statement. The ASMBS made this statement based on the many published studies showing that weight loss surgery is a much more effective treatment for diabetes than medical treatment.
- Gastric banding, sleeve gastrectomy, and gastric bypass have been shown to be well-tolerated and effective treatments for patients with BMI 30 to 35 kg/m2. Safety and efficacy of these procedures in low-BMI patients appear to be similar to results in patients with severe obesity.
Comment from Dr. Oliak – this statement is similar to the previous statement made in 2012. Based on the weight of the published evidence, the ASMBS concluded that weight loss surgery is well-tolerated and effective in low BMI patients.
I encourage you to read the full ASMBS statement to understand the specifics, read a summary of the studies they used in support of their statement, etc. What I’ve written here is just a high-level summary. It’s a PDF, so your device may download it if you click that link.
What the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) has to say
The IFSO, which is the international equivalent of the American Society for Metabolic and Bariatric Surgery (ASMBS), also has published a position statement (in 2014) on weight loss surgery for patients with class 1 obesity (BMI 30-35).
The IFSO position statement recommendations are very similar to the above recommendations by the ASMBS. To summarize, the IFSO recommends (paraphrased):
- Access to bariatric surgery should not be denied to a patient with class I obesity associated simply on the basis of the BMI level. Patients with class I obesity who are not able to achieve adequate weight loss after a reasonable period of nonsurgical therapy should be considered for bariatric surgery.
The full position statement is behind a paywall, but you can read the IFSO position statement abstract.
What the Joint Statement by International Diabetes Organizations has to say
The second Diabetes Surgery Summit, held in 2016, was an international conference that was held to achieve consensus about the benefits and limitations of bariatric surgery for type 2 diabetes. Leading diabetes organizations attended, and the global guidelines they developed were formally endorsed by 45 worldwide medical and scientific societies, including the International Diabetes Federation and the American Diabetes Association.
The recommendations include the following:
- Weight loss surgery should be a recommended option for patients with type 2 diabetes and BMI 40 or greater regardless of level of blood sugar control.
- Weight loss surgery should be a recommended option in patients with poorly controlled type 2 diabetes and BMI 35-39.9
- Weight loss surgery should be considered to be an option in patients with poorly controlled type 2 diabetes and BMI 30-34.9.
Comment from Dr. Oliak – this third recommendation is a strong statement that was agreed upon by the 45 medical, scientific, and diabetes organizations based on many published studies clearly showing the effectiveness of weight loss surgery for the treatment of type 2 diabetes.
The full joint statement is behind a paywall, but you can read the 2nd Diabetes Surgery Summit joint statement abstract.
Key Published Studies on Weight Loss Surgery for Low BMI Patients
Weight Loss Surgery for Patients with BMI 30-35 and Type 2 Diabetes
Many studies show that weight loss surgery is more effective than medical management of diabetes in low BMI people. Here are some of the most important ones:
- Long-term outcomes comparing metabolic surgery to no surgery in patients with type 2 diabetes and body mass index 30-354
Comment from Dr. Oliak – this study showed that weight loss surgery is much better than medical management for the treatment of type 2 diabetes in the BMI 30-35 patient population. Many studies have similarly shown this; the importance of this study is long follow-up. The average follow-up in this study was more than 6 years.
- Lifestyle Intervention and Medical Management With vs Without Roux-en-Y Gastric Bypass and Control of Hemoglobin A1c, LDL Cholesterol, and Systolic Blood Pressure at 5 Years in the Diabetes Surgery Study5
Comment from Dr. Oliak – this study also was a long-term follow-up study (5 years), and also showed that weight loss surgery is much better than medical management for the treatment of type 2 diabetes. Most published studies are short-term follow-up studies, so this study and the above study are important because they show that the short-term benefits of surgery for the treatment of diabetes last long-term, five plus years.
- Bariatric/Metabolic Surgery to Treat Type 2 Diabetes in Patients with a BMI <35 kg/m26
Comment from Dr. Oliak – this is a great study, because it puts together all the data from numerous other studies to make general conclusions. Individual studies often have differing conclusions. When many studies are combined into one, we get the average of what all the published studies show. These types of studies (called meta-analysis studies) are particularly helpful to summarize the entire body of published studies on a given topic.
Gastric Sleeve for Patients with BMI 30-35
Many studies have been published showing that sleeve gastrectomy is safe and effective in the low BMI population. Here are some of the most important ones.
- Is it worth it? Determining the health benefits of sleeve gastrectomy in patients with a body mass index <35 kg/m27
Comment from Dr. Oliak – the quick answer? Yes! This is a great study that looked at all the low BMI patients in Michigan who had the gastric sleeve operation in 2006-2018 (1073 patients). The data showed a high rate of improvement of medical issues (60% of patients off hypertension meds, 64% off insulin, 79% off diabetes oral meds), low complication rates, 72% excess weight loss (EWL) at 1 year, 90% of patients report being “very satisfied”. The study concludes that the operation is safe and effective in the low BMI patient population.
- Sleeve Gastrectomy Outcomes in Patients with BMI Between 30 and 35 – 3 Years of Follow-Up8
Comment from Dr. Oliak – this is a relatively long-term follow-up study (most studies have less than 3 years follow-up) that found low complication rates, no leaks, 83% EWL at 2 years, and a high rate of resolution of weight-related medical issues in 252 low BMI sleeve gastrectomy patients. This study concludes that gastric sleeve surgery is safe and effective in the BMI 30-35 patient population.
- Results of Laparoscopic Sleeve Gastrectomy in 541 Consecutive Patients with Low Baseline Body Mass Index (30-35 kg/m2)9
Comment from Dr. Oliak – This is another great study (541 patients) that shows excellent average weight loss results (78% EWL at 1 year) and low complication rates (leak 0%, bleeding 1.2%) in low BMI people who underwent sleeve gastrectomy surgery. This study also concludes that gastric sleeve surgery is safe and effective in the BMI 30-35 population.
Our Experience with Weight Loss Surgery for Low BMI Patients
We have been performing weight loss surgery for low BMI patients since 2003. We have operated on 260 low BMI patients to date. Currently we mostly do sleeve gastrectomy for low BMI patients, but we also do gastric bypass for low BMI patients with hard-to-control diabetes.
Our experience with sleeve gastrectomy for low BMI patients is similar to the experience reported in the studies quoted above: our weight loss results have been excellent in our low BMI gastric sleeve patients and our complication rates have also been low (leak rate 0%, bleeding 0%).*
Our gastric sleeve surgery weight loss results* (percent of excess weight loss):
- 6mo: 75% EWL
- 9mo: 86% EWL
- 12mo: 88% EWL
- 24mo: 82% EWL
* Individual patient results vary. Patients can lose more or less weight than the averages.
Learn More
Learn more about Orange County bariatric surgeon Dr. Oliak and his Orange County weight loss surgery program.
Bibliography
- Doctors Need to Focus Less on a Patient’s Weight.Scientific American, Feb. 2020, https://www.scientificamerican.com/article/doctors-need-to-focus-less-on-a-patients-weight/
- Brown H. It’s Time to Stop Telling Fat People to Become Thin.Medical Examiner, Mar 24 2015, https://slate.com/technology/2015/03/diets-do-not-work-the-thin-evidence-that-losing-weight-makes-you-healthier.html
- Kaplan LM, Seeley RJ, Harris JL. Myth 1: Weight Can Be Reliably Controlled by Voluntarily Adjusting Energy Balance Through Diet and Exercise. Bariatric Times. 2012;9(4):12-13
- Horwitz D, Padron C, Kelly T, et al. Long-term outcomes comparing metabolic surgery to no surgery in patients with type 2 diabetes and body mass index 30-35. Surg Obes Relat Dis. 2020 Apr;16(4):503-508
- Ikramuddin S, Korner J, Lee WJ, et al. Lifestyle Intervention and Medical Management With vs Without Roux-en-Y Gastric Bypass and Control of Hemoglobin A1c, LDL Cholesterol, and Systolic Blood Pressure at 5 Years in the Diabetes Surgery Study. JAMA. 2018 Jan 16;319(3):266-278
- Cummings DE, Cohen RV. Bariatric/Metabolic Surgery to Treat Type 2 Diabetes in Patients With a BMI <35 kg/m2. Diabetes Care. 2016 Jun;39(6):924-33
- Varban OA, Bonham AJ, Finks JF, et al. Is it worth it? Determining the health benefits of sleeve gastrectomy in patients with a body mass index <35 kg/m2. Surg Obes Relat Dis. 2020 Feb;16(2):248-253
- Berry MA, Urrutia L, Lamoza P, et al. Sleeve Gastrectomy Outcomes in Patients with BMI Between 30 and 35-3 Years of Follow-Up. Obes Surg. 2018 Mar;28(3):649-655
- Noun R, Slim R, Nasr M, et al. Results of Laparoscopic Sleeve Gastrectomy in 541 Consecutive Patients with Low Baseline Body Mass Index (30-35 kg/m2). Obes Surg. 2016 Dec;26(12):2824-2828
More Weight Loss Surgery Resources

David Oliak, M.D.
Dr. Oliak is a board-certified, fellowship-trained surgeon who specializes in minimally invasive (laparoscopic and robotic) weight loss surgery. He has been in practice in Orange County, California, since 2002, has completed more than 3000 weight loss operations, and has a track record of excellent patient outcomes.*
Dr. David Oliak is the founder of the Oliak Center for Weight Loss. He started the Oliak Center because he wanted to provide weight loss surgery done right. His commitment has always been to provide the kind of care that he himself would want to receive. Dr. Oliak is affiliated with only the best bariatric hospitals and surgery centers in Los Angeles County and Orange County.
* Individual patient results vary. Past performance is not a guarantee of future results.
Which weight loss surgeon is right for you?
Download this guide of questions to ask your weight loss surgeon to help make the best decision for you.



