Gastric sleeve surgery
Gastric sleeve surgery (also known as vertical sleeve gastrectomy, vsg, sleeve gastrectomy, or simply sleeve) is the most common weight loss surgery performed in the United States and worldwide. In the US, 75% of first time weight loss operations are gastric sleeve operations. The surgery involves reducing the size of the stomach from approximately 30-40 ounces in volume, to approximately 3-4 ounces in volume. The small stomach enables you to feel satisfied with much smaller food portions.
If you have at least 50 pounds of weight to lose (BMI 30 or greater), sleeve gastrectomy surgery may be the ideal weight loss surgery option for you.
How much weight can you lose after gastric sleeve surgery?
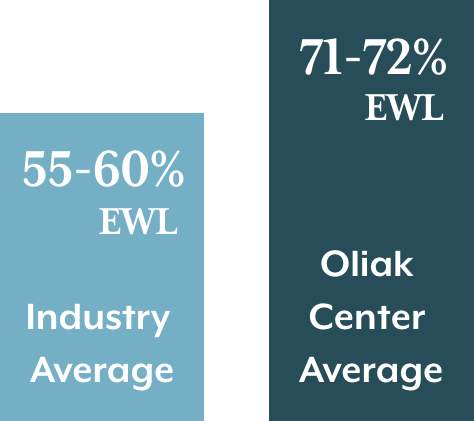
Weight loss after gastric sleeve surgery is typically fast and dramatic, and occurs over 1 - 2 years.* The industry average for weight loss in gastric sleeve patients is 55-60% of their excess weight (%EWL) after surgery.1-2 On average, patients maintain most of their initial weight loss long-term (5+ years), according to published studies.* 2-3
To calculate excess weight, see the MetLife height-weight tables.
Dr. Oliak’s gastric sleeve patients however lose an average of 71-72% of their excess weight after surgery, which beats the industry average by 20%.*
*Individual patient results vary. Patients can lose more or less than the average.
Why are there such big differences in weight loss outcomes?
It’s a lack of standardization across the industry. Surgical details about the dimensions, shape, and size of the sleeve aren’t standardized.4 This means different surgeons do the surgery differently. In fact, a surgeon’s results can even vary greatly between individual operations. Aftercare is also not standardized, so different programs do different things in regards to patient education, follow-up, and support.
Our patients get better outcomes
…because Dr. Oliak has standardized his surgical procedure and weight loss program based on his analysis of the data he gathers about each patient. That’s why our patient outcomes are consistently better than the industry average.*
72%
Average Excess weight loss at 1 year*
72%
Average Excess weight loss at 2 years*
71%
Average Excess weight loss at 3 years*
68%
Average Excess weight loss at 5 years*
* Individual patient results vary. Past performance is not a guarantee of future results.
Why does gastric sleeve surgery work for weight loss?
Gastric sleeve surgery works in two ways for weight loss.
1. The surgery decreases the size of the stomach, which physically restricts the volume of food a patient can consume.
2. The surgery lowers the body weight set point (the biology that regulates body weight).
The body weight set point is the reason why losing weight and maintaining weight loss without surgery is virtually impossible.
When you lose weight through diet and exercise, the body fights to maintain the body weight you previously had. It does this by increasing hunger and decreasing metabolism until you get get back to your set point. And no matter how much you diet and exercise, your body does not lower this set point.5
But weight loss surgery resets the set point to a lower, healthier weight. This means patients feel much more satisfied eating smaller food portions! It’s the combination of smaller stomach size and biology change that makes weight loss surgery work so well.6
Why choose gastric sleeve surgery instead of gastric bypass?
Gastric bypass is the other weight loss surgery that Dr. Oliak performs. Both surgeries result in weight loss and have high rates of patient satisfaction. So why would you want to choose the gastric sleeve surgery instead of the bypass?
The sleeve is often the favored operation for patients with lower initial BMI, and patients without severe diabetes and / or severe or chronic GERD.
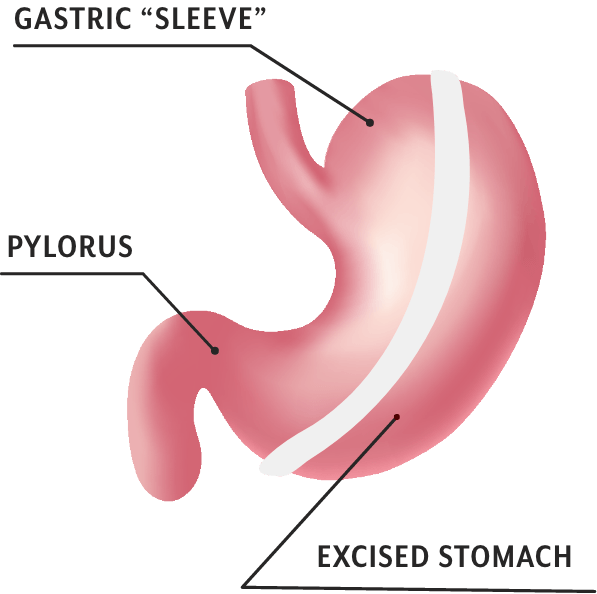
The sleeve gastrectomy operation
Sleeve gastrectomy involves surgically removing a large portion of the stomach, creating a “sleeve” shaped stomach. This reduces stomach volume substantially.
There is no industry-wide standard for the dimensions and volume of the sleeve. Because of this, there is significant variation in how the operation is done from surgeon to surgeon.4
Dr. Oliak, however, uses specific measurements to create a gastric sleeve with exact dimensions and volume. During surgery, he reduces the stomach volume from the typical 30-40 ounces to 3-4 ounces. Over time this volume typically increases to approximately 6-8 ounces. He tailors the measurements to each patient’s specific situation.
The gastric sleeve operation is done laparoscopically or robotically, typically using 5 small incisions. The operation usually takes 1.5-2 hours. Because the gastric sleeve operation is minimally invasive, recovery is generally rapid. Patients typically are discharged from the hospital the day after surgery, and return to work in 1-2 weeks.
Gastric sleeve surgery is only the beginning of successful weight loss
Gastric sleeve patients remain on a liquid diet for 3 weeks after surgery, and then slowly transition to eating progressively more solid foods.
Gastric sleeve surgery is best thought of as a tool that helps you eat less. However, weight loss surgery does not prevent bad eating habits and excess calorie intake. High-calorie foods are still high-calorie foods. Even if you consume less of them, it will still be easy to consume too many calories!
Also, over time, the sleeve naturally expands to approximately 6-8 ounces in volume. This creates more opportunities for eating too many calories. That’s why changing your eating habits is so important for long-term weight loss success.
In the past you failed at this because your body weight set point was too high. But this time will be different, because your body weight set point will be lower. Your biology will be on your side. It will be much easier for you to make the changes your body wouldn’t let you make before.
Follow-up helps ensure you remain on track to reach your goal weight. Because weight loss is so good at the beginning, patients sometimes make the mistake of thinking they don’t need to follow the habit guidelines right away. But being off-track in the beginning can lead to not reaching your long-term weight loss goals. Education and follow-up will help you make the necessary lifestyle changes to get you to your goal weight.
Risks associated with gastric sleeve surgery
Sleeve gastrectomy is considered a safe operation, but complications can occur. Overall, studies clearly show that living with obesity is riskier than having sleeve gastrectomy surgery.
However, complication rates vary across surgeons/programs. One recent, high-quality study showed a 17-fold range in complication rates across 155 accredited bariatric surgery COE (center of excellence) programs nationwide.7 Choosing the right surgeon matters for both getting good weight loss results and minimizing complications.
EARLY COMPLICATIONS - LEAK
Leak is the most feared potential early complication after gastric sleeve surgery. A leak is a hole that develops along the line of division on the stomach before it’s healed.
Leaks typically occur from too much pressure putting strain on the line of division in the stomach, which prevents it from healing properly. This pressure commonly comes from surgical techniques where the sleeve is too narrow in one place, or kinks or twists. When the patient eats or drinks, it results in pressure and potential leak. (Less commonly, leaks can also happen in the case of a patient overeating)
Leaks can largely be prevented with good surgery.
A surgeon’s leak rate can be an excellent measurement of operative technique.
0%
Dr. Oliak’s Gastric Sleeve Leak Rate*
1-2.4%
Industry Average Surgeon Leak Rate8-11
7%
Individual Surgeon Leak Rate CAN BE AS HIGH AS8
Please read Dr. Oliak's blog post Gastric Sleeve Outcomes Vary by Surgeon to learn more about how leak rates vary between individual surgeons.
Late Complications – Acid Reflux
Acid reflux, or GERD (gastroesophageal reflux disease) is the main potential long-term complication after gastric sleeve surgery. Heartburn and other symptoms of post-surgery acid reflux can usually be controlled with diet and/or medication.
There is a large variation in GERD rates across the industry. In Dr. Oliak’s experience, the variation is mostly due to differences in surgical technique and patient behavior. His outcomes data suggest that too narrow of a sleeve causes more GERD, and so does chronic overeating.
A surgeon’s GERD rate can be an excellent measurement of operative technique.
14%
Dr. Oliak’s rate of post-op increased GERD*
19-23%
Industry average rate of post-op increased GERD12
58%
Individual surgeon GERD rate can be as high as12
The Oliak Center for Weight Loss’s GERD rates compare favorably with the published literature. For our patients who have symptoms of GERD, they are typically able to control them with diet and/or medication. Good surgery and good patient care greatly help minimize the risk of post-op GERD.
If you have severe GERD before surgery, you may be a better candidate for gastric bypass surgery.
*Individual patient results vary. Past performance is not a guarantee of future results.
Are you a candidate for gastric sleeve surgery?
Gastric sleeve surgery may be a good option for people who are 50 pounds or more overweight (BMI 30 or greater) and have previously tried and failed to lose weight and keep it off.
Health insurance policies often cover gastric sleeve surgery, but not always. When they do cover surgery, there are strict requirements. Patients must have a BMI of more than 40, or must have a BMI of 35-39 along with diabetes, high blood pressure, or sleep apnea. Patients typically must also complete a 3-6 month medically supervised diet before their insurance will authorize surgery.
Some patients don’t meet their health insurance policy criteria but might still be excellent candidates for sleeve gastrectomy. Some people with low BMI (30-34) and people with BMI 35-39 without serious medical issues (diabetes, high blood pressure, sleep apnea) may still greatly benefit from gastric sleeve surgery.
We provide low BMI gastric sleeve surgery (BMI 30-34) for select patients on a case-by-case basis, which many programs don’t provide.
For patients who don't meet their insurance plan's criteria for surgery, or don't have insurance coverage for weight loss surgery, we offer an established cash-pay program and attractive financing options.
To learn more about gastric sleeve and whether it’s right for you, attend a free, no-obligation educational consultation with Dr. Oliak in Brea or Torrance.
- Fischer L, Hildebrandt C, Bruckner T, et al. Excessive weight loss after sleeve gastrectomy: a systematic review. Obes Surg. 2012 May;22(5):721-31
- Gagner M, Deitel M, Erickson AL, et al. Survey on laparoscopic sleeve gastrectomy (LSG) at the Fourth International Consensus Summit on Sleeve Gastrectomy. Obes Surg. 2013 Dec;23(12):2013-7
- Juodeikis Ž, Brimas G. Long-term results after sleeve gastrectomy: A systematic review. Surg Obes Relat Dis. 2017 Apr;13(4):693-699
- Varban OA, Niemann A, Stricklen A, et al. Far from Standardized: Using Surgical Videos to Identify Variation in Technique for Laparoscopic Sleeve Gastrectomy. J Laparoendosc Adv Surg Tech A. 2017 Aug;27(8):761-767
- Kaplan LM, Seeley RJ, Harris JL. Myth 1: Weight Can Be Reliably Controlled by Voluntarily Adjusting Energy Balance Through Diet and Exercise. Bariatric Times. 2012;9(4):12-13
- Kaplan LM, Seeley RJ, Harris JL. Myth 2: Bariatric Surgery Induces Weight Loss Primarily by Mechanical Restriction and Nutrient Malabsorption. Bariatric Times. 2012;9(4):12-13
- Ibrahim AM, Ghaferi AA, Thumma JR, et al. Variation in Outcomes at Bariatric Surgery Centers of Excellence. JAMA Surg. 2017;152(7):629–636
- Aurora AR, Khaitan L, Saber AA. Sleeve gastrectomy and the risk of leak: a systematic analysis of 4,888 patients. Surg Endosc. 2012;26(6):1509–1515
- Stroh C, Köckerling F, Volker L, et al. Obesity Surgery Working Group, Competence Network Obesity. Results of More Than 11,800 Sleeve Gastrectomies: Data Analysis of the German Bariatric Surgery Registry. Ann Surg. 2016 May;263(5):949-55
- Chang SH, Freeman NLB, Lee JA, et al. Early major complications after bariatric surgery in the USA, 2003-2014: a systematic review and meta-analysis. Obes Rev. 2018 Apr;19(4):529-537
- Gagner M, Kemmeter P. Comparison of laparoscopic sleeve gastrectomy leak rates in five staple-line reinforcement options: a systematic review. Surg Endosc. 2020 Jan;34(1):396-407
- Yeung KTD, Penney N, Ashrafian L, Darzi A, Ashrafian H. Does Sleeve Gastrectomy Expose the Distal Esophagus to Severe Reflux?: A Systematic Review and Meta-analysis. Ann Surg. 2020;271(2):257–265