Gastric bypass surgery
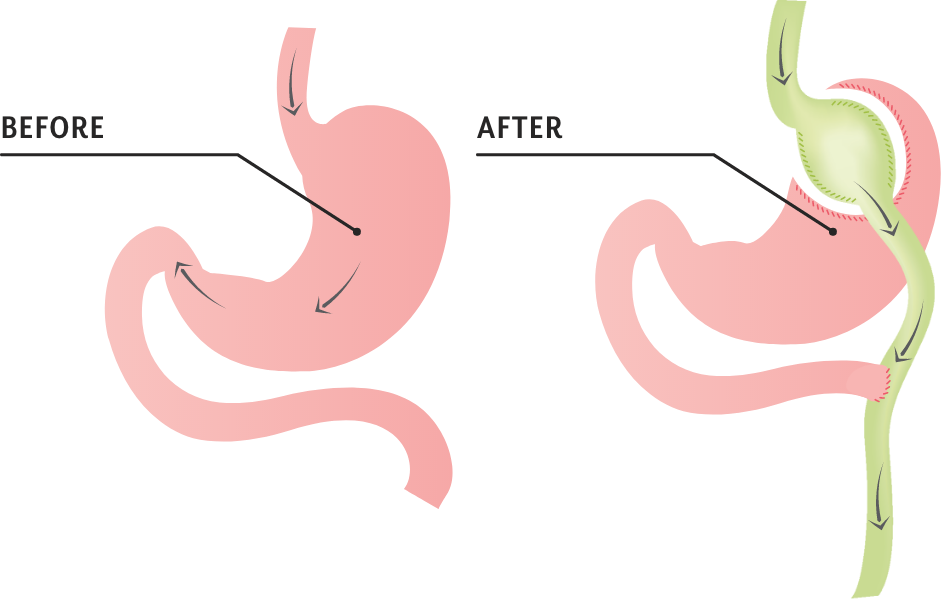
Gastric bypass surgery (also known as roux-en-y gastric bypass, or simply bypass) is the most established and time tested because it has been around for the longest time. The surgery involves creating a small gastric pouch from your stomach that is then connected to your small intestine. When you eat, food travels through the pouch and into the intestine, bypassing most of your stomach (hence the name). The small pouch enables you to feel satisfied with small amounts of food.
If you have at least 75 pounds of weight to lose (BMI 35 or greater), gastric bypass surgery may be the ideal weight loss surgery option for you.
How much weight can you lose after gastric bypass surgery?
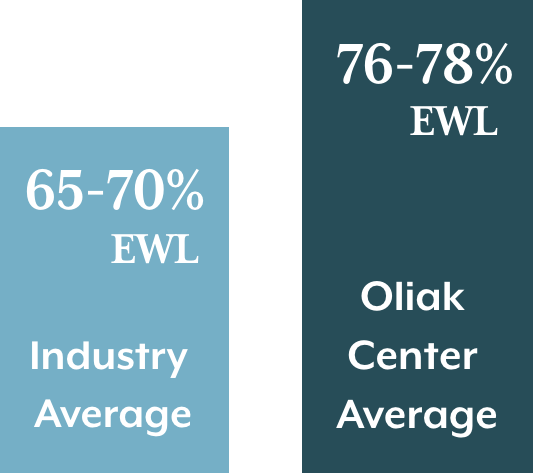
Weight loss after gastric bypass surgery is typically fast and dramatic, and occurs over 1 - 2 years.* The industry average for weight loss in gastric bypass patients is approximately 60-70% EWL (excess weight loss) in 1-3 years after surgery1-3 and 50-60% after 10 years.* 2,4
To calculate ideal weight, see the Metropolitan Life Insurance height-weight tables.
Dr. Oliak’s gastric bypass patients however lose an average of 76-78% of their excess weight at 1-3 years after surgery, and 65% of their excess weight at 10 years after surgery.*
* Individual patient results vary. Patients can lose more or less than the average.
Why are there such big differences in weight loss outcomes?
Because there’s no standardized surgical and aftercare process across the weight loss surgery field. Different surgeons and programs do the operation and aftercare differently, and these differences affect outcomes.
Our patients get better outcomes
...because Dr. Oliak has refined his surgical procedure and weight loss program based on his analysis of the outcomes data he gathers about each patient. That’s why our patient outcomes are consistently better than the industry average.*
76%
Average Excess weight loss at 1 year*
78%
Average Excess weight loss at 2 years*
77%
Average Excess weight loss at 3 years*
72%
Average Excess weight loss at 5 years*
* Individual patient results vary. Past performance is not a guarantee of future results.
Why does gastric bypass surgery work for weight loss?
Gastric bypass surgery results in weight loss for 2 reasons.
1. Gastric bypass decreases the size of the stomach, which physically restricts the volume of food a patient can consume.
2. Gastric bypass lowers the body weight set point (the biology that regulates body weight) by changing the way hormones are released from the GI tract.
The body weight set point is the reason why losing weight and maintaining weight loss without surgery is virtually impossible.
When you lose weight through diet and exercise, the body fights to maintain the body weight you previously had. It does this by increasing hunger and decreasing metabolism until you get get back to your set point. And no matter how much you diet and exercise, your body does not lower this set point.5
But weight loss surgery resets the set point to a lower, healthier weight. This means patients feel much more satisfied eating smaller food portions! It’s the combination of smaller stomach size and biology change that makes weight loss surgery work so well.6
Did you know?
WEIGHT-related medical issues.
Why choose gastric bypass surgery instead of gastric sleeve?
Sleeve gastrectomy is the other weight loss surgery that Dr. Oliak performs. Both surgeries work well for weight loss and have high rates of patient satisfaction. When might a patient opt for gastric bypass surgery instead of gastric sleeve?
The gastric bypass operation is often favored for patients with a higher initial BMI (greater than 50 or 60), severe or poorly controlled diabetes, or severe / chronic GERD. It’s also often the best choice for a bariatric revision (repeat weight loss surgery) operation.
Gastric bypass and diabetes
The effects of gastric bypass surgery on diabetes are profound.
For type 2 diabetics who have had the surgery:
- 75% diabetes remission rate after gastric bypass7
- 22 times more likely to see diabetes abate with weight loss surgery than with diet/exercise alone8
- 70% decrease in death within 7 years9
- 45% decrease in heart attack events within 7 years9
- 52% decrease in stroke events within 7 years9
The American Diabetes Association recommends bariatric surgery be considered for adults with type 2 diabetes who have a BMI greater than 35, in particular if diabetes or associated comorbidities are difficult to control with lifestyle and pharmacologic therapy.10
Additionally, gastric bypass surgery can prevent, improve, or even resolve more than 40 weight-related medical issues.
The gastric bypass operation
Gastric bypass involves surgically creating a very small pouch from the upper part of the stomach, and making a small connection between the stomach pouch and the intestine. As a result, when food is consumed, it passes through the small pouch into the intestine, bypassing the majority of the stomach and the first part of the intestine.
There is no industry-wide standard for the details of the operation (dimensions and volume of the stomach pouch, size/method for pouch/intestine connection, and intestine lengths). Because of this, there is significant variation in how the operation is done from surgeon to surgeon.
Dr. Oliak, however, uses specific measurements to create a very small stomach pouch and small connection between the pouch and intestine. His measurements are based on 15+ years of patient data, and his outcomes for weight loss and complications are better than typical industry results.*
The gastric bypass operation is done laparoscopically or robotically, typically using 5 small incisions. The operation usually takes about 2 hours and recovery is generally rapid. Patients typically are discharged from the hospital 1-2 days after surgery, and return to work in approximately 2 weeks.*
* Individual patient results vary.
Gastric bypass surgery is only the beginning of successful weight loss
Gastric bypass patients remain on a liquid-only diet for several weeks after surgery, and then slowly transition to eating progressively more solid foods.
Gastric bypass surgery is best thought of as a “tool” that helps you eat less. However, weight loss surgery does not prevent bad eating habits and excess calorie intake. High-calorie foods are still high-calorie foods. Even if you consume less of them, it may still add up to too many calories!
Also, over time, the pouch becomes more efficient at emptying, resulting in the ability to eat larger portion sizes. This creates more opportunity for eating too many calories. That’s why maintaining good eating habits is so important for long-term weight loss success.
In the past you failed at this because your body weight set point was too high. But this time will be different, because your body weight set point will be lower. Your biology will be on your side. It will be much easier for you to make the changes your body wouldn’t let you make before.
Follow-up helps ensure you remain on track to reach your goal weight. Because weight loss is so good at the beginning, patients sometimes make the mistake of thinking they don’t need to follow the habit guidelines right away. But being off-track in the beginning can lead to not reaching your long-term weight loss goals. Education and follow-up will help you make the necessary lifestyle changes to get you to your goal weight.
Risks associated with gastric bypass surgery
Gastric bypass surgery has a 40+ year track record of being a safe operation. However, complications can occur. Overall, studies clearly show that living with obesity is riskier than having gastric bypass surgery.
However, complication rates vary across surgeons/programs. One recent large study showed a 17-fold range in complication rates across 155 accredited bariatric surgery COE (center of excellence) programs nationwide.11 Choosing the right surgeon matters for both getting good weight loss results and minimizing complications.
EARLY COMPLICATIONS
Potential serious early complications include blood clots and leaks. The risk for both can be minimized, but not totally eliminated.
- Blood clots are risks with all operations. But walking frequently after surgery (every 1-2 hours while awake for at least 1 month) lowers the risk for blood clots. Studies report the risk to get a blood clot after gastric bypass surgery for an average risk patient to be approximately 0.5%.12
- Leaks are a risk with any operation that involves cutting across the stomach or intestine. A leak is a hole that develops along the stomach pouch or intestine before it’s healed. Leaks typically occur as a result of surgical technique. Put another way, leaks can be mostly prevented with a good operation and patient care.
A surgeon’s leak rate can be an excellent measurement of operative technique.
0.2%
Dr. Oliak’s Gastric Bypass Leak Rate (5-10x Less Than Industry Average)*
1% - 2%
Average Surgeon Gastric Bypass Leak Rate13-14
Late Complications
Because of the way the gastric bypass surgery changes the GI tract, there are several potential long-term complications that can occur (that are different from the gastric sleeve surgery). These include vitamin/mineral deficiencies, low blood sugar, alcohol addiction, bowel obstruction, and ulcer.
A good surgery and patient care can minimize these issues, but not completely eliminate them.
*Individual patient results vary. Past performance is not a guarantee of future results.
Are you a candidate for gastric bypass surgery?
Gastric bypass candidates are generally at least 75-100 pounds overweight (BMI 35 or greater), and have tried and failed to lose weight and keep it off.
Health insurance policies often cover weight loss surgery, but not always. When they do cover weight loss surgery, there are strict requirements. Patients must have a BMI of more than 40, or must have a BMI of 35-39 along with diabetes, high blood pressure, or sleep apnea. Patients usually must also complete a 3-6 month medically supervised diet before their health insurance will authorize surgery.
Some patients may still be good candidates for gastric bypass surgery even if they don't meet their insurance criteria. Examples include patients with BMI 35-39 who don’t have the severity of medical issues required by their insurance. Some people with low BMI (30-34) who have severe type 2 diabetes and poor blood sugar control may also benefit from gastric bypass surgery.
For patients who don't meet their insurance plan's criteria for weight loss surgery, or don't have insurance coverage for weight loss surgery, we offer a cash pay program and attractive financing options.
Wondering if gastric bypass is right for you? We offer free, no-obligation consultations with Dr. Oliak. Set up your appointment today!
- Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: A systematic review and meta-analysis. J Am Med Assoc. 2004;292:1724-1737
- O'Brien PE, McPhail T, Chaston TB, et al. Systematic review of medium-term weight loss after bariatric operations. Obesity Surgery. 2006;16:1032-1040
- Puzziferri N, Roshek TB 3rd, Mayo HG, et al. Long-term follow-up after bariatric surgery: a systematic review. JAMA. 2014 Sep 3;312(9):934-42
- O'Brien P, McDonald L, Anderson M, et al. Long term outcomes after bariatric surgery: Fifteen year follow up after gastric banding and a systematic review of the literature. Ann Surg. 2013;257:87-94
- Kaplan LM, Seeley RJ, Harris JL. Myth 1: Weight Can Be Reliably Controlled by Voluntarily Adjusting Energy Balance Through Diet and Exercise. Bariatric Times. 2012;9(4):12-13
- Kaplan LM, Seeley RJ, Harris JL. Myth 2: Bariatric Surgery Induces Weight Loss Primarily by Mechanical Restriction and Nutrient Malabsorption. Bariatric Times. 2012;9(4):12-13
- Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366(17):1577–1585
- Gloy VL, Briel M, Bhatt DL, et al. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJ. 2013 Oct 22;347:f5934
- Fisher DP, Johnson E, Haneuse S, et al. Association Between Bariatric Surgery and Macrovascular Disease Outcomes in Patients With Type 2 Diabetes and Severe Obesity. JAMA. 2018 Oct 16;320(15):1570-1582
- American Diabetes Association. Obesity management for the treatment of type 2 diabetes. Sec. 7. In Standards of Medical Care in Diabetes - 2017. Diabetes Care 2017; 40(Suppl. 1):S57–S63
- Ibrahim AM, Ghaferi AA, Thumma JR, Dimick JB. Variation in Outcomes at Bariatric Surgery Centers of Excellence. JAMA Surg. 2017;152(7):629–636
- Flum DR, Belle SH, King WC, et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 2009 Jul 30;361(5):445-54
- Zellmer JD, Mathiason MA, Kallies KJ, et al. Is laparoscopic sleeve gastrectomy a lower risk bariatric procedure compared with laparoscopic Roux-en-Y gastric bypass? A meta-analysis. Am J Surg. 2014;208(6):903–910
- Chang SH, Freeman NLB, Lee JA, et al. Early major complications after bariatric surgery in the USA, 2003-2014: a systematic review and meta-analysis. Obes Rev. 2018;19(4):529–537