In previous posts I’ve discussed why weight loss surgery works (Weight Loss Surgery Changes The Body Weight Set Point) and why diets don’t work (The Body Weight Set Point Prevents Weight Loss). To summarize, bariatric surgery works by changing the biologic control system that determines body weight. The biologically determined body weight “set point” is decreased. Diets on the other hand almost never work long-term because they do not change the biologically determined body weight set point.
Based on our emerging understanding of the unique ability of surgery to change the biology that determines body weight, the justification for surgery as a treatment for obesity has never been stronger. Clearly the potential benefits of surgery are substantial, but what are the actual surgery outcomes?
Outcomes include surgical outcomes – mortality, complications – and weight loss outcomes – how much weight loss, failure rate, regain rate, etc. Also, what role do patients and surgeons play in achieving good or bad outcomes?
Weight Loss Surgery Safety – Mortality
In this post I will discuss the most important weight loss surgery safety measure – mortality after weight loss surgery. In future posts I will discuss the other outcomes topics listed above.
All operations have a mortality rate. Surgical mortality is generally defined as mortality occurring within 30 days of surgery. Some operations have a low 30-day mortality rate and some have a high 30-day mortality rate. Mortality rate is determined by the complexity of the operation and the sickness of the patients undergoing the operation.
Examples of low mortality rate operations include gallbladder removal (0.3-0.5%), appendix removal (0.1-0.4%), and hysterectomy (0.1-0.6%). Examples of higher mortality rate operations include heart bypass surgery (2-3.5%) and colon cancer surgery (6%).
Before I further discuss weight loss surgery safety I should explain where we get the numbers.
High Quality Weight Loss Surgery Patient Databases
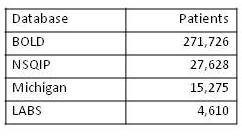
In the field of bariatric surgery there are several high quality multicenter databases containing large numbers of patients. These databases were begun within the last several years and now contain meaningful data. The databases and the number of patients within each database, as of mid 2012, are as follows:
The BOLD database is the ASMBS (American Society for Metabolic and Bariatric Surgery) Center of Excellence (COE) database, the NSQIP database is the ACS (American College of Surgeons) COE database, the Michigan database includes virtually all patients who undergo bariatric surgery in Michigan, and LABS is an ongoing prospective multicenter outcomes study.
An important point to make is that these databases include large numbers of patients from many different hospitals and from many different surgeons. Before we had these data, our outcomes data largely came from individual case series published by individual surgeons. These types of studies generally show good results (because the surgeon wouldn’t publish his results if they were not good!), but they do not necessarily reflect the actual outcomes achieved throughout the population. For this reason large multicenter databases like those above are of very high value.
Weight Loss Surgery Mortality Rates Very Low
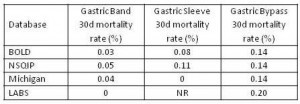
So what are the mortality rates after LAP-BAND®, sleeve gastrectomy, and gastric bypass surgery? See the table below for 30-day mortality rates for each operation in each of the databases:
The first point to make is that the mortality rates after LAP-BAND®, gastric sleeve, and gastric bypass are all very low. These mortality rates (0.03-0.2%) compare favorably to the mortality rates for other operations that are considered safe such as gallbladder removal (0.3-0.5%), appendix removal (0.1-0.4%), and hysterectomy (0.1-0.6%). This is impressive given the fact that many bariatric patients are considered high risk due to multiple medical problems such as diabetes and sleep apnea.
The second point to make is that the mortality rates differ between the three bariatric operations. The band has the lowest mortality rate (approx 1 in 2500) and the Gastric Bypass has the highest mortality rate (approx 1 in 750). The Sleeve Gastrectomy has a mortality rate between that for the bypass and band (approx 1 in 1000).
In conclusion, we now have accurate weight loss surgery mortality data from multiple, large, multicenter databases containing more than 300,000 patients. These data demonstrate impressively low mortality rates after LAP-BAND®, sleeve gastrectomy, and gastric bypass surgery. Bariatric surgery mortality rates are similar to mortality rates for other operations regarded as safe, such as gallbladder removal, appendectomy, and hysterectomy.
Read more about Dr. Oliak and his Orange County weight loss surgery program at www.OliakCenter.com.
More Weight Loss Surgery Resources

David Oliak, M.D.
Dr. Oliak is a board-certified, fellowship-trained surgeon who specializes in minimally invasive (laparoscopic and robotic) weight loss surgery. He has been in practice in Orange County, California, since 2002, has completed more than 3000 weight loss operations, and has a track record of excellent patient outcomes.*
Dr. David Oliak is the founder of the Oliak Center for Weight Loss. He started the Oliak Center because he wanted to provide weight loss surgery done right. His commitment has always been to provide the kind of care that he himself would want to receive. Dr. Oliak is affiliated with only the best bariatric hospitals and surgery centers in Los Angeles County and Orange County.
* Individual patient results vary. Past performance is not a guarantee of future results.
Which weight loss surgeon is right for you?
Download this guide of questions to ask your weight loss surgeon to help make the best decision for you.