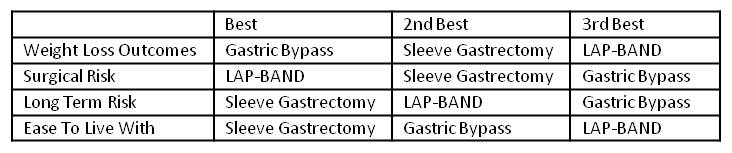
Three parameters that are important to consider when deciding between gastric sleeve, gastric bypass, and LAP-BAND® are weight loss outcomes, risk, and impact on lifestyle.
Weight Loss Outcomes
Weight loss outcomes on average are better with gastric bypass and sleeve gastrectomy than LAP-BAND®. There are two reasons for this.
First, gastric bypass and sleeve gastrectomy are restrictive; that is, they force very small portions on patients, particularly early (first 1-2 years) after surgery. This is because the stomach is made smaller – about 1-2 ounces for the bypass and 3-4 ounces for the sleeve. This forced behavior modification helps patients to lose significant weight.
The LAP-BAND® procedure is not restrictive in the same way because the stomach is not reduced in size. The stomach is segmented into two sections by the band, but the overall size of the stomach is unchanged. Because of this, portion control after the band is more of a voluntary behavior change than after the gastric bypass or sleeve gastrectomy.
Second, gastric bypass and sleeve gastrectomy are more effective at “resetting” the body weight “set point” to a lower weight. See Dr. Oliak’s blog post’s The Body Weight Set Point Prevents Weight Loss, and Weight Loss Surgery Changes The Body Weight Set Point. This, in effect, makes the body “want” to weigh a lower weight, and makes maintenance of weight loss possible long-term.
The LAP-BAND® works differently. The LAP-BAND® helps to suppress hunger with less food. This makes weight loss easier to accomplish. This is great, but it is not the same as resetting the set-point lower. With the band, weight loss is more dependent on voluntary behavior change than the bypass or the sleeve.
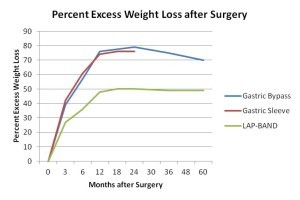
For these reasons average weight loss outcomes are better with the gastric bypass and sleeve gastrectomy than with the LAP-BAND® (see graph below of our weight loss data). Average weight loss is approximately 60-80% of excess weight after the sleeve and bypass, and 40-50% of excess weight after the band. Disclaimer – these statistics are averages, individual patients can lose more or less weight than the average.
What weight loss statistics like these don’t convey is how much variation there is around the average. With LAP-BAND® there is substantial variation around the average – some patients do a lot better than the average, and some do a lot worse. With the gastric bypass and sleeve gastrectomy there is less variation around the average. Most gastric bypass and gastric sleeve patients lose 60-80% of their excess weight over the first 1-3 years. Disclaimer – Individual patient results vary with the LAP-BAND®, gastric bypass, and sleeve gastrectomy.
Between the gastric bypass and the sleeve gastrectomy, the bypass wins the outcomes comparison by a hair. It is the more established (>40 years) and well studied operation, and it is the better operation for diabetes. The sleeve, though, places a very close second. The LAP-BAND® places a distant third.
Risk
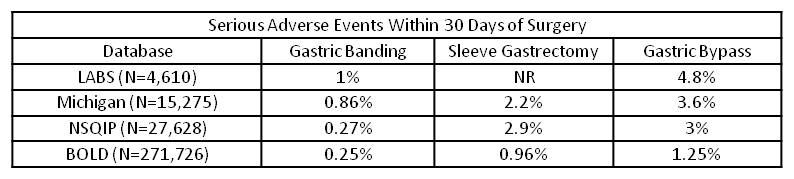
There are two types of risk to consider. The first is the initial surgical risk, which is the risk of having a complication due to undergoing the operation. This risk is quantified as the rate of complications that occur within 30 days of surgery.
The second type of risk is long-term risk. This risk is quantified as the rate of complications that occur >30 days after surgery.
Initial surgical risk corresponds with the invasiveness of the operation. Surgical risk is therefore lowest with the LAP-BAND®, higher with the sleeve, and highest with the bypass.
As you can see in the table below, the chance for a serious complication within 30 days of surgery is about 1% after the band, 2-3% after the sleeve, and 3-5% after the bypass. These numbers are all considered low. See Dr. Oliak’s post Weight Loss Surgery Is Safe. Disclaimer – Individual patient results vary.
Long-term risk (>30 days postop) is lowest after the sleeve gastrectomy. This is because GI tract anatomy remains essentially normal (except for the much smaller stomach). There is ongoing risk after the band because of the presence of the band (a foreign body), and after the gastric bypass because of the rerouting of the GI tract.
In the risk category, the LAP-BAND® wins for lowest early postoperative risk, and the sleeve wins for lowest long-term risk.
Impact on Lifestyle
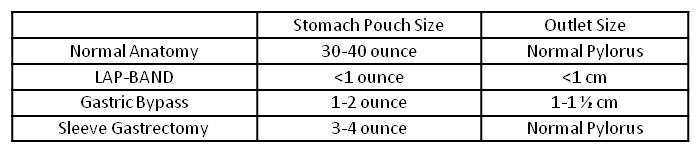
Weight loss surgery will impact your lifestyle by changing how you are able to eat. The magnitude of this impact depends on the magnitude of the surgical change – the smaller the stomach pouch and the smaller the pouch outlet, the bigger the impact.
Think for a moment about normal anatomy. The stomach is typically 30-40 ounces in size, and empties through a sphincter (pylorus) that can open wide or close completely. This anatomy, as we all know, is not very limiting in terms of how we are able to eat.
Now think about how surgery alters this normal anatomy (see table below). Each operation involves reconfiguring the stomach into a much smaller stomach pouch. The band and bypass also involve constructing a small outlet so food can exit the pouch.
These surgical changes will require you to take small bites, chew well, and eat slowly. The bypass and sleeve will restrict your portion sizes.
Because the LAP-BAND® has the smallest pouch size (<1 ounce) and the smallest outlet size (<1 cm), it will impact how you will be able to eat the most. This makes the LAP-BAND® the hardest of the three operations to live with day to day.
Gastric bypass is easier to live with than the LAP-BAND® because the stomach pouch size and outlet size are larger.
Sleeve gastrectomy is the easiest of the three operations to live with because the pouch is the largest (3-4 ounces) and the pouch outlet is the normal pylorus, which can open wide or close completely. This combination of a larger pouch and the normal pylorus makes eating after surgery similar to eating before surgery, except regarding portion sizes. Disclaimer – Individual patient results vary.
Conclusion
Important parameters to consider when choosing gastric sleeve, gastric bypass, or LAP-BAND® are outcomes, risk, and impact on lifestyle.
Read more about Dr. Oliak and his Orange County weight loss surgery program at www.OliakCenter.com.
More Weight Loss Surgery Resources

David Oliak, M.D.
Dr. Oliak is a board-certified, fellowship-trained surgeon who specializes in minimally invasive (laparoscopic and robotic) weight loss surgery. He has been in practice in Orange County, California, since 2002, has completed more than 3000 weight loss operations, and has a track record of excellent patient outcomes.*
Dr. David Oliak is the founder of the Oliak Center for Weight Loss. He started the Oliak Center because he wanted to provide weight loss surgery done right. His commitment has always been to provide the kind of care that he himself would want to receive. Dr. Oliak is affiliated with only the best bariatric hospitals and surgery centers in Los Angeles County and Orange County.
* Individual patient results vary. Past performance is not a guarantee of future results.
Which weight loss surgeon is right for you?
Download this guide of questions to ask your weight loss surgeon to help make the best decision for you.